‘Antibiotic resistance’ is the ability of bacteria or other microbes to resist the effects of an antibiotic. Such problem must be faced squarely in every country where they can take actions that will benefit everybody. Actually, antibiotic resistance can affect anyone, of any age, in any country. This problem has become one of the world’s most pressing public health problems. Antibiotic resistance is increasing at an alarming rate.
A growing list of infections i.e., pneumonia, tuberculosis, and gonorrhea are becoming harder and at times impossible to treat while antibiotics are becoming less effective. Antibiotic-resistant infections correlate with the level of antibiotic consumption. Non-judicial use of antibiotics is mostly responsible for making the microbes resistant. ‘Antibiotics’, also known as ‘antimicrobial drugs’, are drugs that fight infections caused by bacteria. After the first use of antibiotics in the 1940s, they transformed medical care and dramatically reduced illness and death from infectious diseases.
The term ‘antibiotic’ originally referred to a natural compound, as penicillin or streptomycin, produced by various microorganisms, having the capacity to inhibit the growth of or to destroy bacteria and other microorganisms, used chiefly in the treatment of infectious diseases. However, some antibiotics may be synthetic (produced by chemical synthesis) or semi-synthetic (produced by a microbe that is subsequently modified by chemical synthesis) that can also kill or inhibit the growth of microbes.
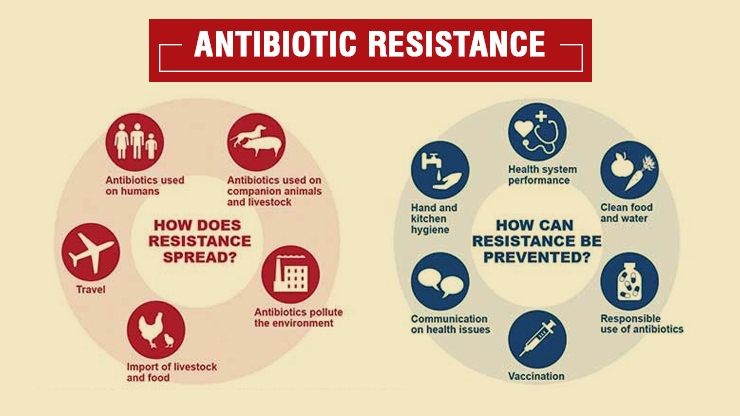
Antibiotic resistance occurs when bacteria change in some way that reduces or eliminates the effectiveness of antibiotics to cure or prevent infections. These antibiotic resistant bacteria can quickly spread to society – threatening the community with a new strain responsible for infectious disease that is more difficult to cure and more expensive to treat. For this reason, antibiotic resistance is among ‘The Centers for Disease Control and Prevention’ (CDC)’s top concerns. Someone with a bacterium that is resistant to a certain medicine can pass that resistant bacterium to another person. In this way, a hard-to-treat illness can be spread from person to person. In some cases, the illness can lead to serious disability or even death. Mechanisms of resistance – Bacteria can become resistant to antibiotics through several mechanisms. Some bacteria develop the ability to neutralize the antibiotic before it can do harm, others can rapidly pump the antibiotic out, and still others can change the antibiotic attack site, so it cannot affect the function of the bacteria. Ultimately, the resistant bacteria survive and continue to multiply. As a result, they replace all the bacteria that were killed off causing more harm to the patient who is infected with that bacteria.
In addition, bacteria that were at one time susceptible to an antibiotic can acquire resistance through mutation (mutations are alterations to a DNA sequence.) of their genetic material or by one of the methods of genetic transfer. The biochemical mechanisms of resistance may be several, including decreased permeability to the drug, development of alternative metabolic pathways, and production of enzymes inactivating the drug. The DNA that codes for resistance can be grouped in a single easily transferable package. Thus, that bacterium becomes resistant to many antimicrobial agents because of the transfer of one piece of DNA. If a microbe is resistant to many drugs, treating the infections it causes can become very difficult or even impossible.
Prevention and Control – Resistance to an antibiotic develops in no time and hence, is a big matter of concern. With the improvement of technology, more people are now aware of the ill-effects caused by resistance to the available drugs, however, very few take proactive steps to curb the resistance by not over using the antibiotics. Evidence from the literature suggests that the knowledge regarding antibiotic resistance in the population is still scarce. In the developing world, almost all the antibiotics are available over the counter and can be bought without any medical prescription which is one of the most important factors in causing the resistance. Therefore, if the resistance to the antibiotics needs to be curbed, the only way shall be to educate the general public. To aware the common people, experts suggest to follow some guidelines to prevent/control the menace of antibiotic resistance: i) Only antibiotics can be used when they are prescribed by a certified health professional. ii) For a viral infection, antibiotics should not be taken. iii) After completion of the prescribed course of treatment, any leftover medication should be discarded. iv) Doses of the prescribed antibiotic should not be skipped. v) The prescribed course of treatment should be completed, even if the patient feels better. If treatment stops suddenly, some bacteria may become resistant and reinfect. vi) Antibiotics prescribed for someone else, should not be taken by others. Since the same antibiotic may not be appropriate for others. In this manner, taking wrong medicine may delay correct treatment which will allow bacteria to multiply. Considering the ill-effects of antibiotic resistance, the health professionals across the globe discuss to significantly prevent/control the problem. Accordingly, a Global Action Plan on Antimicrobial Resistance, including antibiotic resistance, was endorsed at the World Health Assembly in May 2015.
In addition to CDC and Global Action Plan, WHO is also leading multiple initiatives to address a common problem, i.e., antimicrobial resistance. A UN report issued on drug resistance says that drug-resistant diseases could kill 10 million people a year by 2050. Antibiotic resistance is at all time high in all the parts of the world. Despite measures taken by some member states of WHO, antibiotic use in humans is increasing. The high economic burden in the healthcare sector has become a burning issue, due to extended hospital stays, isolation wards, stringent infection control measures and treatment failures. For antibiotic resistance, a surveillance system coordinated at national and international levels, ongoing analysis and a mandatory reporting system should be established by health professionals. Both domestic and global policies need to be conventional and adhered-to to stop the overuse and misuse of antibiotics.











 6 Sep 2021
6 Sep 2021



